Although Omar Wood has a clinical background in nursing and is a certified surgical first assistant, his role at Gresham Smith speaks to a broader purpose. As the firm’s first hire in clinical advisory services, Omar brings decades of healthcare operations experience to design pursuits, working in close partnership with project executives, clients, and design teams to guide operational strategy and optimize care environments through data-informed decision-making.
We recently sat down with Omar to learn more about his unique role as clinical liaison, how he supports our Healthcare design practice, and what trends he’s watching as the industry evolves.


Your role as Clinical Liaison is quite unique. Can you share what your day to day looks like?
Omar Wood: At Gresham Smith, I serve as a clinical liaison within Advisory Services, which means I help healthcare clients, specifically hospital leadership, make more strategic decisions around operations, master planning, and resourcing. That might involve looking at clinical workflow, utilization data, or staffing models to support smarter capital projects. By understanding a client’s long-term goals and challenges, I can recommend operational improvements that may reduce the need for expansion—or at least ensure it’s done in the most efficient way possible.
I’m often studying data to uncover inefficiencies. For example, if a hospital is at 60% capacity, but wants to increase its capacity to achieve revenue goals, I may review metrics and propose revised staffing models or scheduling shifts instead of suggesting immediate buildouts. I help clients define the best path forward by aligning clinical operations with design strategy.
How does your healthcare background influence client support and design collaboration?
Omar: Having worked as a nurse and surgical first assistant, I understand firsthand what it’s like to navigate poorly designed spaces—I’ve been the clinician on the ground. That experience gives me a unique lens into how design affects safety, care quality, and staff satisfaction. I’ve worked in nearly every department in a hospital, particularly the OR and emergency department, so I understand operational demands. For example, I know that OR turnover times have real financial impact. By improving workflows and reducing room reset times, we can potentially generate additional revenue and improve staff morale.
All of that helps me collaborate more effectively with our design teams in evaluating clinical workflows, defining room adjacencies, or creating staffing efficiencies that support broader operational goals.
“By understanding a client’s long-term goals and challenges, I can recommend operational improvements that may reduce the need for expansion—or at least ensure it’s done in the most efficient way possible.”
What inspired your transition into this role, and what drew you to Gresham Smith?
Omar: I’ve really been bridging this gap informally for more than 20 years—working in healthcare consulting, medical equipment planning, and operations efficiency. In earlier roles, I’d walk through departments, sit like a fly on the wall, and talk to staff about what was or wasn’t working. I’ve always enjoyed problem-solving and driving systems improvements.
When I decided to formalize that work in a clinical advisory role, I was already familiar with Gresham Smith through past collaboration and knew the firm to be a leader in healthcare design. The opportunity to help build this function from the ground up was compelling and aligned perfectly with my skill sets.
Can you share a project where your involvement made a meaningful impact?
Omar: One example from my work that stands out, prior to joining Gresham Smith, involved an operating room we were supporting that was consistently operating in the red. By optimizing workflow, streamlining vendor contracts, and aligning staff capabilities with demand, we carved out tangible savings that increased revenue, enabling the hospital to reinvest in capital equipment upgrades.
That change resulted in better patient outcomes, greater employee satisfaction, and stronger financial performance. The domino effect was real—improve one metric and you unlock opportunities throughout the entire care environment.

You mentioned being a bridge between clinicians and designers—how do you collaborate with project teams internally?
Omar: That’s a really important part of the role. Doug Spies [Advisory Services program director and a senior vice president in Gresham Smith’s Healthcare practice] and I are currently touring our Healthcare offices to introduce this service line internally. While many of our project executives and designers understand the value of clinical input conceptually, they may not be aware of how to integrate it into pursuits or project development. I want them to see me as a partner early in the process—not just when something’s broken.
Even if the client doesn’t need a full operational analysis, I can support spatial planning and workflow efficiency at the design level. We’ve created heat maps to show the burden of movement on clinical staff and recommend layouts that reduce fatigue and enhance productivity. It’s about advocating for the end user while still helping us win work and excel in delivery.
“… That’s when my bridging role really comes into play: I can translate clinician feedback into actionable design recommendations, and vice versa, helping both sides understand and align.”
What challenges have you faced translating clinical needs into design terms?
Omar: One big challenge is communication. Clinicians aren’t always familiar with reading architectural drawings in 2D —so when we present concepts without something tangible, it’s hard for them to visualize the impact. That’s when my bridging role really comes into play: I can translate clinician feedback into actionable design recommendations, and vice versa, helping both sides understand and align.
You also have to manage personalities and time constraints. Many providers are under pressure and short-staffed. Listening actively, reading the room, and navigating those dynamics is vital to making progress.
What trends in healthcare should design teams be tracking more closely, and how are you helping to connect those dots?
Omar: Artificial intelligence [AI] is definitely changing the landscape—from data visualization to predictive modeling. While I’m not a designer, I work closely with our Research & Insights team and people like Matt Harrell [Gresham Smith’s Data Analytics leader] who are developing proprietary analytics tools to help clients see their challenges and opportunities more clearly. Visual dashboards and decision-support tools are game changers, helping our teams respond more quickly and strategically.
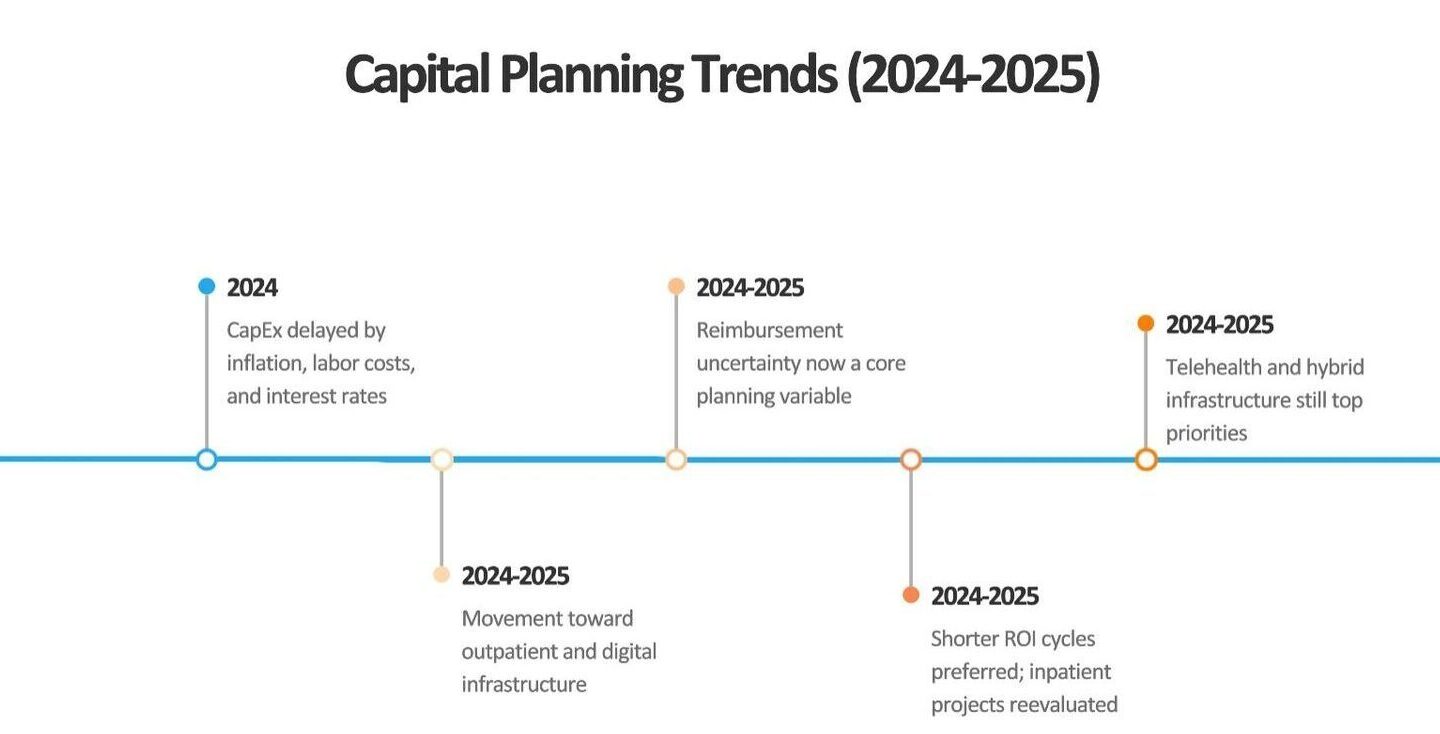
I also think we need to continue focusing on operational flexibility. The future of healthcare is all about adaptability—facilities need to respond not just to the next pandemic, but to shifting models of care and demographic needs. That’s where advisory services can provide real foresight—especially when it comes to capital planning. Understanding long-term investment priorities and aligning them with evolving care delivery models is key.
“More and more, clients are looking for partners who can connect financial, clinical, and operational goals—not just deliver beautiful buildings…”
Looking ahead, how do you see the Clinical Liaison role evolving in A/E firms?
Omar: I believe this role will become foundational. More and more, clients are looking for partners who can connect financial, clinical, and operational goals—not just deliver beautiful buildings. The availability of data—and the ability to interpret it for real strategy—is driving change across the board. If we, as A/E firms, want to compete with larger players and offer more value, this is how we differentiate ourselves.
At the same time, nothing I do is proprietary. Our value will come from being thought leaders, trusted collaborators, and advocates for meaningful, measurable solutions.

How does your role connect back to Gresham Smith’s Core Purpose to plan, design and consult to create healthy and thriving communities?
Omar: To build better communities, you’ve got to start by creating facilities where people want to work and receive care. I’ve worked in settings where poor design directly impacted morale, effectiveness, and safety. I understand those pressures—and bringing that lived experience into planning ensures we’re designing spaces that actually function.
When we work from the inside out—combining empathy, data, and strategy—we position our clients and our communities for long-term success. That’s truly what keeps me motivated.













